We serve Chemical Name:(1-Phenyl-4-piperidinyl)methanol CAS:697306-45-9 to global customers since 2007, Pls send inquiry to info@nbinno.com or visit www.nbinno.com our official website should you have any interests. This site is for information only.
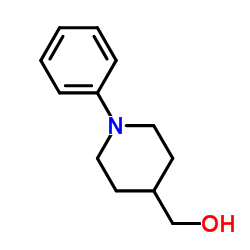
Chemical Name:(1-Phenyl-4-piperidinyl)methanol
CAS.NO:697306-45-9
Synonyms:(1-phenyl-4-piperidyl)methan-1-ol;(1-Phenyl-4-piperidyl)methanol;1-Phenyl-4-piperidinemethanol;4-Piperidinemethanol, 1-phenyl-;(1-Phenyl-4-piperidinyl)methanol;4-Piperidinemethanol,1-phenyl;T6NTJ AR& D1Q;(1-phenyl-piperidin-4-yl)-methanol
Molecular Formula:C12H17NO
Molecular Weight:191.270
HS Code:2933399090
Physical and Chemical Properties:
Melting point:N/A
Boiling point:327.2±15.0 °C at 760 mmHg
Density:1.1±0.1 g/cm3
Index of Refraction:1.548
PSA:23.47000
Exact Mass:191.131012
LogP:1.68
Material Safety Information (Applicable for Hazard Chemicals)
RIDADR:
Packing Group:
Contact us for information like (1-phenyl-4-piperidyl)methan-1-ol chemical properties,Structure,melting point,boiling point,density,molecular formula,molecular weight,(1-phenyl-piperidin-4-yl)-methanol physical properties,toxicity information,customs codes,safety, risk, hazard and MSDS, CAS,cas number,4-Piperidinemethanol, 1-phenyl- Use and application,T6NTJ AR& technical grade,usp/ep/jp grade.
Related News: Fate Therapeutics�� iPSC product platform is supported by an intellectual property portfolio of over 250 issued patents and 150 pending patent applications. (1-Phenyl-4-piperidinyl)methanol manufacturer Also, the study did not compare people who had COVID-19 with those who did not, to see if such symptoms were higher than in the general population. The report did exclude patients with certain serious or chronic preexisting conditions like cancer, kidney disease, HIV, liver disease and stroke, to separate their previous health status from post-COVID symptoms. (1-Phenyl-4-piperidinyl)methanol supplier China has asked the European Union for help in buying urgently needed medical supplies from its member countries, the China��s official Xinhua news agency said on Saturday. (1-Phenyl-4-piperidinyl)methanol vendor The Basser Center launched its initiative Black & BRCA” in 2020 to bring tailored resources and support to the Black community for genetic counseling and testing.
“At a time when Black men and women are more likely to be diagnosed with cancer at later stages when it is less treatable, Black & BRCA seeks to empower people to understand their family health history and take action to prevent cancer from one generation to the next,” Domchek said.
Suffering through a case of COVID-19 unleashed a host of other health problems in hundreds of thousands of Americans participating in the largest study yet of the long-term effects of coronavirus infection.
Tracking the health insurance records of nearly 2 million people who caught the coronavirus last year, researchers found that one month or more after their infection, almost one-quarter of them sought medical treatment for new conditions, The New York Times reported.
The range of both those affected and the symptoms that struck them was wide. The health issues affected all ages, including children. The most common new health problems were pain; breathing difficulties; high cholesterol; malaise and fatigue; and high blood pressure. But symptoms did not stop there: Some suffered intestinal symptoms; migraines; skin problems; heart abnormalities; sleep disorders; and mental health conditions like anxiety and depression.
Post-COVID health problems did not spare those who had not been seriously ill: While nearly half of patients who were hospitalized for COVID-19 experienced subsequent medical issues, so did 27 percent of people who had mild or moderate symptoms and 19 percent of people who said they were asymptomatic.
“One thing that was surprising to us was the large percentage of asymptomatic patients that are in that category of long COVID,” Robin Gelburd, president of the nonprofit FAIR Health, told the Times.
Gelburd said that since asymptomatic people can have post-COVID symptoms, patients and doctors alike should consider the possibility that some health issues may actually be aftereffects of coronavirus infection.
In total, the report found that more than 454,000 people consulted health providers for symptoms 30 days or more after their infection. The analysis was evaluated by an independent academic reviewer but was not formally peer-reviewed, according to FAIR Health.
“The strength of this study is really its size and its ability to look across the range of disease severity in a diversity of age groups,” Dr. Helen Chu, an associate professor of medicine and infectious diseases at the University of Washington’s School of Medicine, told the Times.
The report “drives home the point that long COVID can affect nearly every organ system,” Dr. Ziyad Al-Aly, chief of the research and development service at the VA St. Louis Health Care System, told the Times.
“Some of these manifestations are chronic conditions that will last a lifetime and will forever scar some individuals and families,” added Al-Aly, who authored a large study published in April on lingering symptoms in COVID-19 patients in the Department of Veterans Affairs health system.
In the latest report, the most common issue for which patients sought medical care was pain — including nerve inflammation and aches and pains associated with nerves and muscles. It was reported by more than a fifth of those who reported post-COVID problems. Breathing difficulties, including shortness of breath, were experienced by 3.5 percent of post-COVID patients.
Nearly 3 percent of patients sought treatment for symptoms that were labeled with diagnostic codes for malaise and fatigue, a far-reaching category that could include issues like brain fog and exhaustion that worsens after physical or mental activity, the Times reported.
The database included only people with private health insurance or Medicare Advantage, not those uninsured or covered by Medicare Parts A, B and D, Medicaid or other government health programs. Chu told the Times that people without insurance or with incomes low enough to qualify for Medicaid are often “more likely to have worse outcomes. (1-Phenyl-4-piperidinyl)methanol factory Also, the study did not compare people who had COVID-19 with those who did not, to see if such symptoms were higher than in the general population. The report did exclude patients with certain serious or chronic preexisting conditions like cancer, kidney disease, HIV, liver disease and stroke, to separate their previous health status from post-COVID symptoms.
“At a time when Black men and women are more likely to be diagnosed with cancer at later stages when it is less treatable, Black & BRCA seeks to empower people to understand their family health history and take action to prevent cancer from one generation to the next,” Domchek said.
Suffering through a case of COVID-19 unleashed a host of other health problems in hundreds of thousands of Americans participating in the largest study yet of the long-term effects of coronavirus infection.
Tracking the health insurance records of nearly 2 million people who caught the coronavirus last year, researchers found that one month or more after their infection, almost one-quarter of them sought medical treatment for new conditions, The New York Times reported.
The range of both those affected and the symptoms that struck them was wide. The health issues affected all ages, including children. The most common new health problems were pain; breathing difficulties; high cholesterol; malaise and fatigue; and high blood pressure. But symptoms did not stop there: Some suffered intestinal symptoms; migraines; skin problems; heart abnormalities; sleep disorders; and mental health conditions like anxiety and depression.
Post-COVID health problems did not spare those who had not been seriously ill: While nearly half of patients who were hospitalized for COVID-19 experienced subsequent medical issues, so did 27 percent of people who had mild or moderate symptoms and 19 percent of people who said they were asymptomatic.
“One thing that was surprising to us was the large percentage of asymptomatic patients that are in that category of long COVID,” Robin Gelburd, president of the nonprofit FAIR Health, told the Times.
Gelburd said that since asymptomatic people can have post-COVID symptoms, patients and doctors alike should consider the possibility that some health issues may actually be aftereffects of coronavirus infection.
In total, the report found that more than 454,000 people consulted health providers for symptoms 30 days or more after their infection. The analysis was evaluated by an independent academic reviewer but was not formally peer-reviewed, according to FAIR Health.
“The strength of this study is really its size and its ability to look across the range of disease severity in a diversity of age groups,” Dr. Helen Chu, an associate professor of medicine and infectious diseases at the University of Washington’s School of Medicine, told the Times.
The report “drives home the point that long COVID can affect nearly every organ system,” Dr. Ziyad Al-Aly, chief of the research and development service at the VA St. Louis Health Care System, told the Times.
“Some of these manifestations are chronic conditions that will last a lifetime and will forever scar some individuals and families,” added Al-Aly, who authored a large study published in April on lingering symptoms in COVID-19 patients in the Department of Veterans Affairs health system.
In the latest report, the most common issue for which patients sought medical care was pain — including nerve inflammation and aches and pains associated with nerves and muscles. It was reported by more than a fifth of those who reported post-COVID problems. Breathing difficulties, including shortness of breath, were experienced by 3.5 percent of post-COVID patients.
Nearly 3 percent of patients sought treatment for symptoms that were labeled with diagnostic codes for malaise and fatigue, a far-reaching category that could include issues like brain fog and exhaustion that worsens after physical or mental activity, the Times reported.
The database included only people with private health insurance or Medicare Advantage, not those uninsured or covered by Medicare Parts A, B and D, Medicaid or other government health programs. Chu told the Times that people without insurance or with incomes low enough to qualify for Medicaid are often “more likely to have worse outcomes. (1-Phenyl-4-piperidinyl)methanol factory Also, the study did not compare people who had COVID-19 with those who did not, to see if such symptoms were higher than in the general population. The report did exclude patients with certain serious or chronic preexisting conditions like cancer, kidney disease, HIV, liver disease and stroke, to separate their previous health status from post-COVID symptoms.

